In September 2024, PRM published research proving the effectiveness of the PRM Protocol™ alongside a multimodal approach in treating the symptoms of vaginismus.
The primary objective of this study was to evaluate the impact of the PRM Protocol™ on a wide range of outcome parameters, including:
- Pain
- Functionality
- Work productivity
- Quality of life
- Mental health
- Sexual health
- Healthcare system utilization
It is noteworthy that the participants in this study reported an average pain duration of 9.5 years, underscoring the chronic and debilitating nature of vaginismus.
What is vaginismus?
Vaginismus is a sexual health condition characterized by involuntary muscle spasms or contractions of the pelvic floor muscles surrounding the vagina. These spasms can make any form of vaginal penetration, including sexual intercourse, gynecological examinations, or tampon insertion, painful or even impossible.

It is important to note that vaginismus is not a conscious choice or a result of psychological resistance; instead, it is an involuntary physiological response. With the limited research available on the condition today, it is estimated that somewhere between 5-17% of women are affected.
PRM’s Study for Treating Vaginismus
The study included 961 participants aged 18 to 76 years old diagnosed with vaginismus who sought treatment at an outpatient pelvic rehabilitation practice between April 2021 and December 2022.
The treatment, the patented PRM Protocol™, involved pre-medication with diclofenac 75 mg PO, pre-treatment with a topical anesthetic spray, and weekly external ultrasound-guided trigger point injections of Lidocaine 1% into the pelvic musculature. A global injection targeted specific muscles of the levator ani sling using a flexible, 6‐inch, 27‐gauge needle injected from the subgluteal posterior approach under ultrasound guidance.
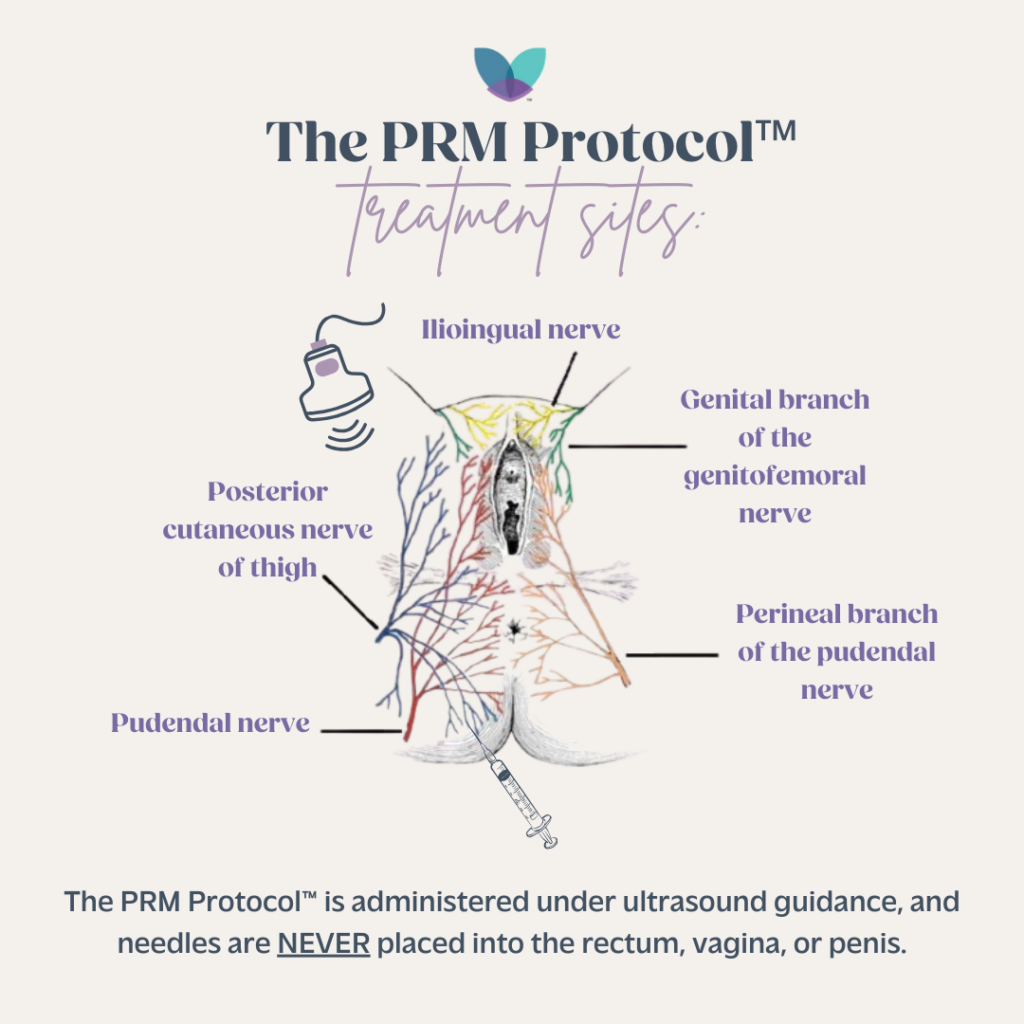
Simultaneous ultrasound‐guided peripheral nerve blocks of the pudendal nerve at Alcock’s canal and the posterior femoral cutaneous nerve were administered. The initial treatment included dexamethasone with Lidocaine 1%, followed by subsequent appointments with normal saline and Lidocaine 1% for nerve blocks. Patients resumed normal activities immediately after treatment.
Along with receiving treatment through the PRM Protocol™, patients did pelvic floor physical therapy either at a local clinic or at home virtually, with the goal of downtraining the pelvic floor musculature and the peripheral and central nervous systems. Patients also simultaneously participated in mindfulness, meditation, and deep breathing exercises at home alone or through PRM’s mindfulness meditation course, Retrain Your Pelvic Pain.
Learn more about the PRM Protocol™
Study Outcomes Relating to Pain and Function
Six weeks after the final treatment, participant response to the PRM Protocol™ was measured.
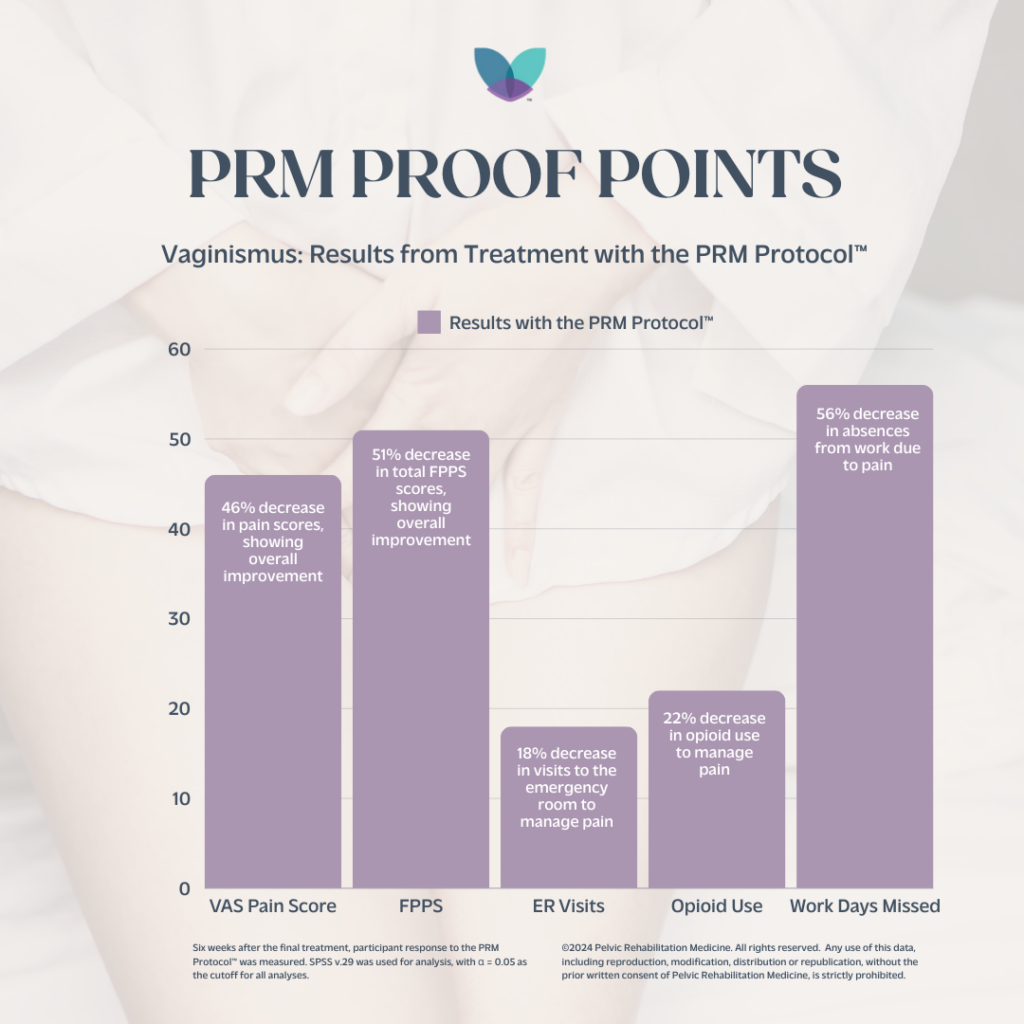
- VAS pain levels decreased by 46%
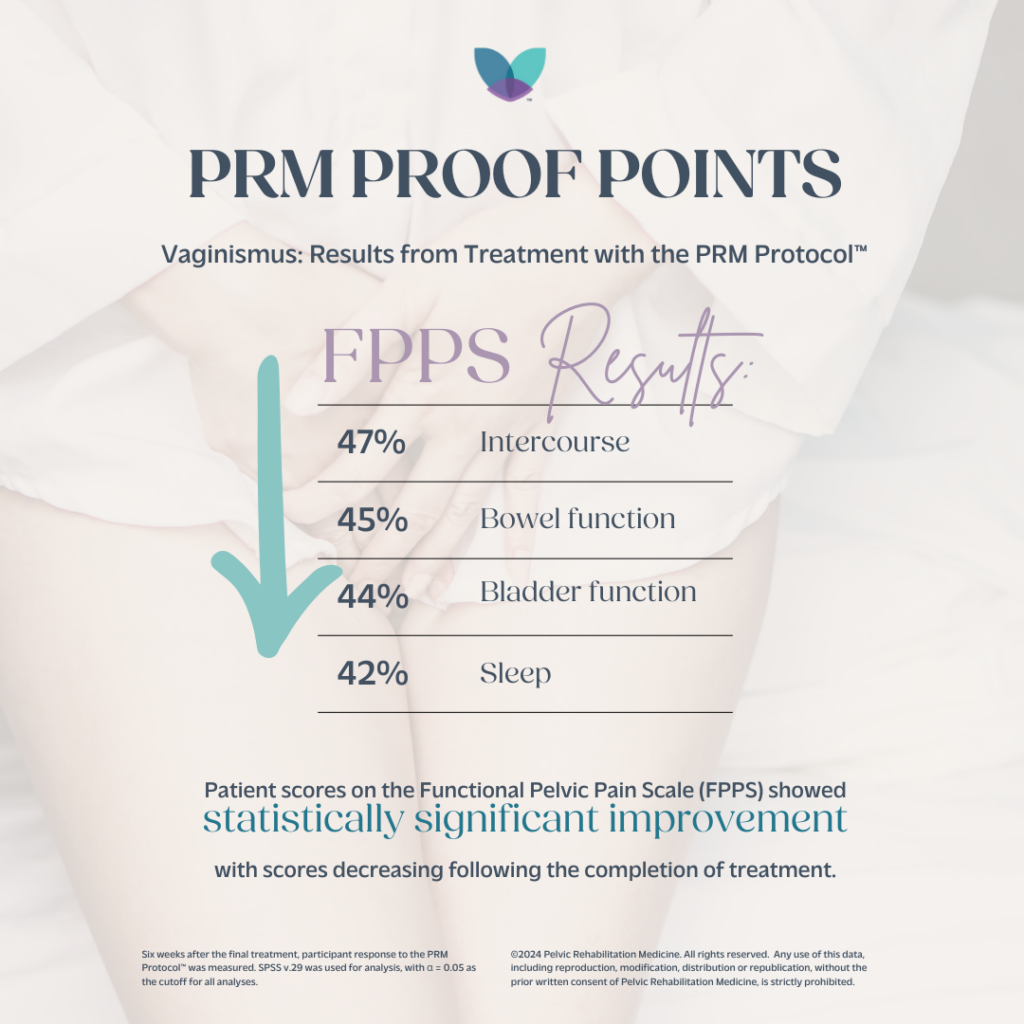
- FPPS total scores decreased by 51%
Improvements in all FPPS categories were statistically significant, with the largest decreases:
- Intercourse (47%)
- Bowel function (45%)
- Bladder function (44%)
- Sleep (42%).
Based on questions asked to patients, asking them to describe their pain and discomfort during sexual activity, results showed that there was an average improvement of 25% in the past 30 days.
Study Outcomes Relating to Productivity and
For those who underwent the PRM Protocol™:
- 38% of patients reported using opioids for their vaginismus-related pain at their first appointment
- 29% of patients reported having gone to an Emergency Room for their vaginismus-related pain at their first appointment.
- These proportions reduced to 16% and 11%, respectively, at their six-week follow-up appointment after undergoing the PRM Protocol™.
- This is a 22% decrease in opioid use and 18% decrease in patients visiting the ER for the treatment group
- Absenteeism, defined by at least one day of work missed in the past three months due to pelvic pain, decreased by 56%.
- Presenteeism, defined by at least 1 hour of work productivity being disturbed by pelvic pain in the past three months, decreased by 68%.
The multimodal treatment approach, addressing both the physical and psychological dimensions of vaginismus, demonstrated a notable degree of success and safety, accompanied by a low recurrence rate. Significantly, the outcomes revealed that this comprehensive approach achieved pain-free intercourse successfully, even for patients with a history of long-term failures with alternative vaginismus treatments. The most notable enhancements were observed in symptoms related to intercourse, sleeping, and bladder function.
The PRM Protocol™ specifically targets pelvic nerve inflammation and the pelvic muscles associated with both intercourse and vaginismus, leading to a reversal of pelvic neurogenic inflammation and a reduction in hypertonic pelvic floor conditions. This, in turn, results in decreased vulvar pain and improved functionality during intercourse.
How does the PRM Protocol™ work in treating vaginismus?
Significant improvements in Visual Analog Scale (VAS) pain levels were observed among patients, underscoring the efficacy of this approach in addressing the fundamental causes of nerve and muscle dysfunction. Myofascial dysfunction in the pelvic region is intricately linked to issues such as bowel, bladder, and sexual dysfunction, contributing to pelvic pain through the presence of myofascial trigger points.
The PRM Protocol™ employs ultrasound-guided trigger point injections in each muscle of the levator ani-sling to address the underlying myofascial pain and pelvic floor dysfunction. This intervention alleviates ongoing nociception, creating space for enhanced flow of pelvic peripheral nerves with reduced constriction and improved blood circulation.
Additionally, the PRM Protocol™ targets both peripheral and central sensitization, aiming to mitigate neurogenic inflammation, inhibit feedback loops from the peripheral to central nervous systems, and prevent cross-sensitization between the pudendal and posterior femoral cutaneous nerves. Peripheral sensitization is managed through consecutive peripheral nerve blocks targeting the pudendal and posterior femoral cutaneous nerves.

The PRM Protocol™ employs two primary mechanisms for this purpose: 1) the reduction of neurogenic inflammation by locally administering dexamethasone to deplete substance P8 and utilizing repeated exposure to lidocaine 1%, which diminishes histamine release from mast cells, and 2) the desensitization of hyperactive peripheral nociceptors through repeated exposure to lidocaine 1%.
In addition to addressing peripheral sensitization, the PRM Protocol™ also focuses on central sensitization by treating associated pelvic neurogenic inflammation, effectively interrupting the feedback loop from the peripheral nervous system to the central nervous system.
It is crucial to note that the overlap in pain patterns and innervation between the pudendal and posterior femoral cutaneous nerves may lead to cross-sensitization, a phenomenon observed in the pelvic region where a sensitized structure can influence an adjacent, otherwise normal structure. The PRM Protocol’s™ multi-faceted approach, addressing myofascial dysfunction, pelvic floor dysfunction, and peripheral and central sensitization, demonstrates a comprehensive strategy for managing the intricate facets of vaginismus.
Conclusion
It is crucial for the medical community to collaboratively establish a streamlined diagnostic and treatment protocol for vaginismus patients, benefiting both the individuals suffering from the condition and the healthcare system. Future research in a university context may address these limitations and contribute to a more comprehensive understanding of the studied phenomenon.
Nevertheless, the findings from this study contribute valuable insights into the potential effectiveness and safety of the PRM Protocol™ in managing vaginismus, presenting a promising avenue for future research and clinical applications. As a complex and multifaceted condition, vaginismus necessitates a comprehensive and compassionate approach for successful diagnosis and treatment. Increased awareness among healthcare providers, coupled with open communication and support, can contribute to improved outcomes for individuals affected by vaginismus.
Ongoing research and advocacy efforts are essential to destigmatize the condition, facilitate early intervention, and enhance the overall well-being of those living with vaginismus.
If you are experiencing the symptoms of vaginismus and have not yet found relief, we encourage your to meet with a pelvic pain specialist to have your symptoms evaluated.
Authors:
Allyson Shrikhande
Lolasri Rampally
Katherine Wolfrum
Rachael Haverland
Kimberlee Leishear
Neha James
Madhu Bagaria
Marjorie Mamsaang
Yogita Tailor
Sandra Sandhu-Restaino
Erika Moody
Jessica Ray
Natalia Obzejta
Laura Brott
Janaki Natarajan
Gautam Shrikhande
