by Dr. Madhu Bagaria, MD, FACOG, Endometriosis Excision Surgeon in New York and New Jersey

What is endometriosis excision surgery, and how does it differ from other surgical treatments for endometriosis?
Endometriosis excision surgery is a surgical procedure performed to cut out the endometriotic lesions from the pelvic cavity and other locations. Unlike other endo surgeries that destroy the implant (ablation), excision aims to completely remove the lesion in entirety.
The benefits of excision surgery is it has potentially lower recurrence rate compared to ablation and has improved pain relief.
It can involve extensive dissection and need a skilled surgeon who is capable of identifying and removing all the lesions.

Other endometriosis surgery include ablation where the tissues are just burned on the surface without removing the actual lesion. So this lesion is still present. Patients may find initial relief in their symptoms but these symptoms come back as the lesions have not been removed. It does not need skilled surgeons and can be done by general OBGYN. When patients have endometriomas or chocolate cyst of the ovaries, they are usually drained but the cyst wall is left behind. Again since the disease portion has not been removed, they do come back.
Learn more about endometriosis excision surgery
Which organs are most commonly affected by endometriosis, and why might they need to be removed or partially removed during surgery?
Endometriosis most commonly affects organs within the pelvis (peritoneum, uterosacrals, ovaries) , though in rare cases it can spread beyond these areas and involve any where from lungs, diaphragm, small and large bowels, appendix, abdominal wall, bladder)
Frequently involved organs include the following:
Ovaries
Endometriosis can form cysts called endometriomas within the ovaries. These cysts can cause pain and disrupt ovarian function. In severe cases, an ovary may be partially removed if the endometrioma is large and deeply embedded, or if there’s significant damage to healthy ovarian tissue.
Fallopian tubes
Endometriosis implants can block or damage the fallopian tubes, hindering egg transport and potentially impacting fertility. During surgery, if the implant is on the surface, this will be removed to enable a complete excision procedure for the best outcome. Sometimes if the tube is diseased or dilated, recommendation is to remove the tube as diseased tube can affect the fertility.
Uterosacral ligaments
These ligaments support the uterus. Endometriosis implants here can cause pain during menstruation or intercourse. The surgeon might remove or excise parts of these ligaments if endometriosis has infiltrated them significantly.
Peritoneum
This is the lining of the pelvic cavity. Endometriosis implants here can cause inflammation and pain. The goal of surgery is to remove these implants.
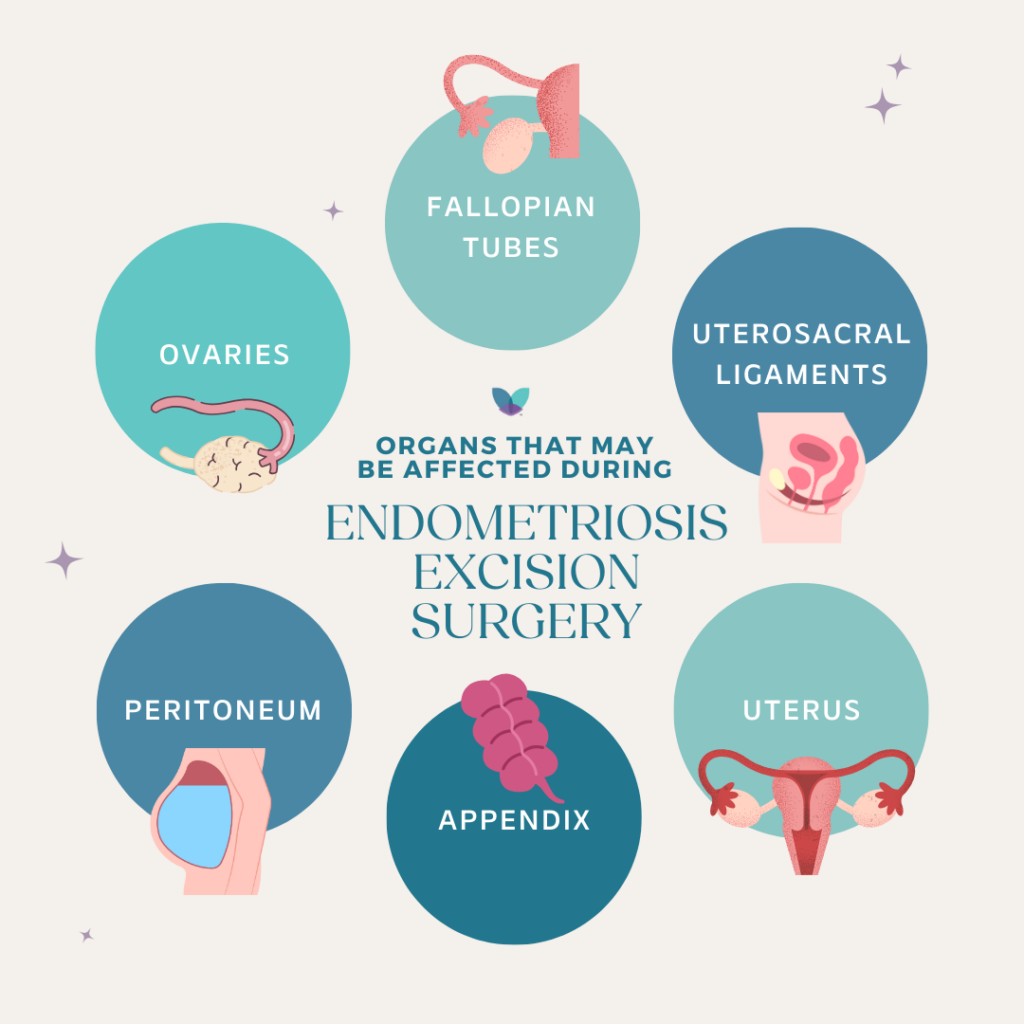
Other organs (less common)
In rare instances, endometriosis can affect the bladder, bowels, or even the diaphragm. If endometriosis implants are found on these organs, the surgeon will attempt to remove them while minimizing damage to healthy tissue. When they are superficial, they can be peeled off from the surface minimizing damage to them. Sometimes a portion of them may need to be removed.
Appendix
It is part of the small bowel and is frequently involved. It is recommended to remove this if involved. Sometimes in young patients and especially someone with extensive endometriosis disease, the appendix should be removed even if it is normal looking.
Uterus
Sometimes especially if fertility is not the goal, in order to completely excise the disease, uterus removal may be necessary in bad adhesive disease involving the bowels and uterus, cervix.
It’s important to remember that the goal of surgery, particularly excision surgery, is meticulously cutting out the endometrial implants themselves, including their roots, while preserving as much healthy tissue as possible. This is why excision surgery is often preferred over ablation techniques that destroy the implants but might leave behind microscopic disease or damage surrounding tissues.
Learn more about endometriosis excision surgery at PRM
What are the risks and benefits associated with removing or partially removing organs during endometriosis excision surgery?
Any surgery has risks and benefits. Endometriosis surgeries are always geared for organ and nerve preservation and the decision to remove or partially remove a portion of an organ is driven by the goal of excising the disease completely to have the best benefit and outcomes.
Risks of incomplete surgery include persistence of pain and high recurrence rate. Other risks include decrease in ovarian reserve (for any endometrioma removal which can sometimes excise a healthy portion of ovaries), temporary change in bowel habits (after resection and re anastomosis of large bowel surgery), damage to hypogastric nerves (if nerves are entrapped in endometriosis). Removal of the appendix is well tolerated. Sometimes a portion of the vagina or bladder is also removed if the nodule is involving the vagina or the bladder. These are well tolerated. With bladder surgery you may be asked to have a temporary Foley catheter which drains the bladder.
Schedule a Consultation with a PRM Surgeon
How can patients prepare for the possibility of organ removal during endometriosis excision surgery?
Here are some ways in which patients can prepare for the surgery.
Pre-surgical Discussions:
- Open Communication with your Doctor: The most crucial step is having an honest and open conversation with your surgeon before the surgery. Discuss the severity and location of your endometriosis, and your individual risk factors for needing an organ removal like appendix, endometrioma cyst removal, removal of portion of bowel, and your preferences regarding fertility and future pregnancies and bowel surgeries.
- Understanding the Options and discussing risks and benefits: Ask your doctor to explain the different scenarios that could necessitate partial organ removal during surgery. This could involve removing a portion of the ovary, removing a section of the uterosacral ligament.
- Second Opinion: If you feel unsure or have concerns, don’t hesitate to seek a second opinion from another qualified endometriosis specialist.
Emotional Preparation:
- Acknowledge Your Feelings: The possibility of organ removal, even partial, can be emotionally challenging. Allow yourself to feel and process your emotions.
- Support System: Lean on your partner, family, friends, or a therapist for support as you navigate this process. Talking to others who have been through similar experiences can be helpful.
- Research and Education: Knowledge is empowering. Research endometriosis surgery and the different potential outcomes to feel more prepared.
What is the recovery process like after endometriosis excision surgery, particularly if organs have been removed or partially removed?
Recovery after endometriosis surgery can vary depending on the type of surgery performed, the extent of endometriosis removal, and your individual healing process.
- Laparoscopic surgery has a shorter recovery time over 4-6 weeks.
- Post-surgical discomfort like pain , discomfort, shoulder pain, fatigue, nausea can be experienced during the recovery process.
- With removal of superficial disease involving any organs, hysterectomy, removal of appendix, cyst of ovaries or removal of tubes- patients are able to go home.
- With deeper implants involving diaphragm or with rectum or bladder your doctor will advise you to stay in hospital for a day or two.
- You may be discharged home with Foley catheter if any bowel or ureteral surgeries are done.
- Certain activity restrictions may be advised like pelvic rest for 6-8 weeks after removal of uterus or portion of vagina.
- Dietary restrictions may be given especially after bowel surgeries.
Follow your doctor’s advice and don’t hesitate to reach out if you have any questions.
